Gum disease is a common and sometimes neglected condition that affects many individuals. It is caused by the accumulation of plaque, a sticky film of bacteria, which can lead to inflammation of the tissue surrounding the teeth, known as the gums. When left untreated, this inflammation can progress into more severe conditions, potentially leading to tooth loss and other health complications. Therefore, healing gum disease starts with a comprehensive understanding of its causes, symptoms, and the necessary steps to prevent and treat the condition.
Managing gum disease involves a combination of professional dental care and strict oral hygiene practices. Dentists can offer specific treatments and interventions to control the infection and regenerate damaged tissue. Daily routines, such as brushing and flossing, become critical in removing plaque and reducing bacteria in the mouth. Additionally, lifestyle and dietary modifications can improve overall oral health and assist in the healing process. When conventional methods are not enough, surgical options may be considered to restore the integrity of the gums and prevent tooth loss.
Key Takeaways
- Effective gum disease management combines professional treatment with daily oral hygiene.
- Reducing plaque buildup is essential to prevent and control gum disease.
- Regular dental check-ups are critical for early diagnosis and intervention.
Understanding Gum Disease
Gum disease, also known as periodontal disease, is a significant dental condition that can affect overall oral health, leading from inflammation to bone loss if left untreated.
Stages of Gum Disease
- Gingivitis: This initial stage is characterized by inflammation of the gums caused by plaque buildup. It’s the body’s natural response to the presence of harmful bacteria.
- Periodontitis: Untreated gingivitis can advance to periodontitis, where the inner layer of gum and bone pull away from the teeth and form pockets. These small spaces between teeth and gums collect debris and can become infected.
Causes and Risk Factors
- Plaque Accumulation: The primary cause of gum disease is plaque, a sticky film of food debris, bacteria, and saliva. If plaque is not removed, it turns into tartar which is harder to clean.
- Tobacco Use: Smoking is significantly associated with the onset and progression of gum disease.
- Health Conditions: Conditions like diabetes can increase the risk of developing gum diseases.
- Genetics: One may be genetically predisposed to periodontal disease, making them more susceptible to it.
Recognizing the Symptoms
- Symptoms of Gum Disease: Persistent bad breath, red or swollen gums, tender or bleeding gums, and painful chewing.
- Visual Clues: Teeth that look longer due to recession of the gums or visible pockets between teeth and gums can be signs of advancing periodontal disease.
Professional Diagnosis
When diagnosing gum disease, dental professionals conduct a thorough examination to assess the health of the gums and teeth. This process involves specific steps to determine the presence and severity of the condition.
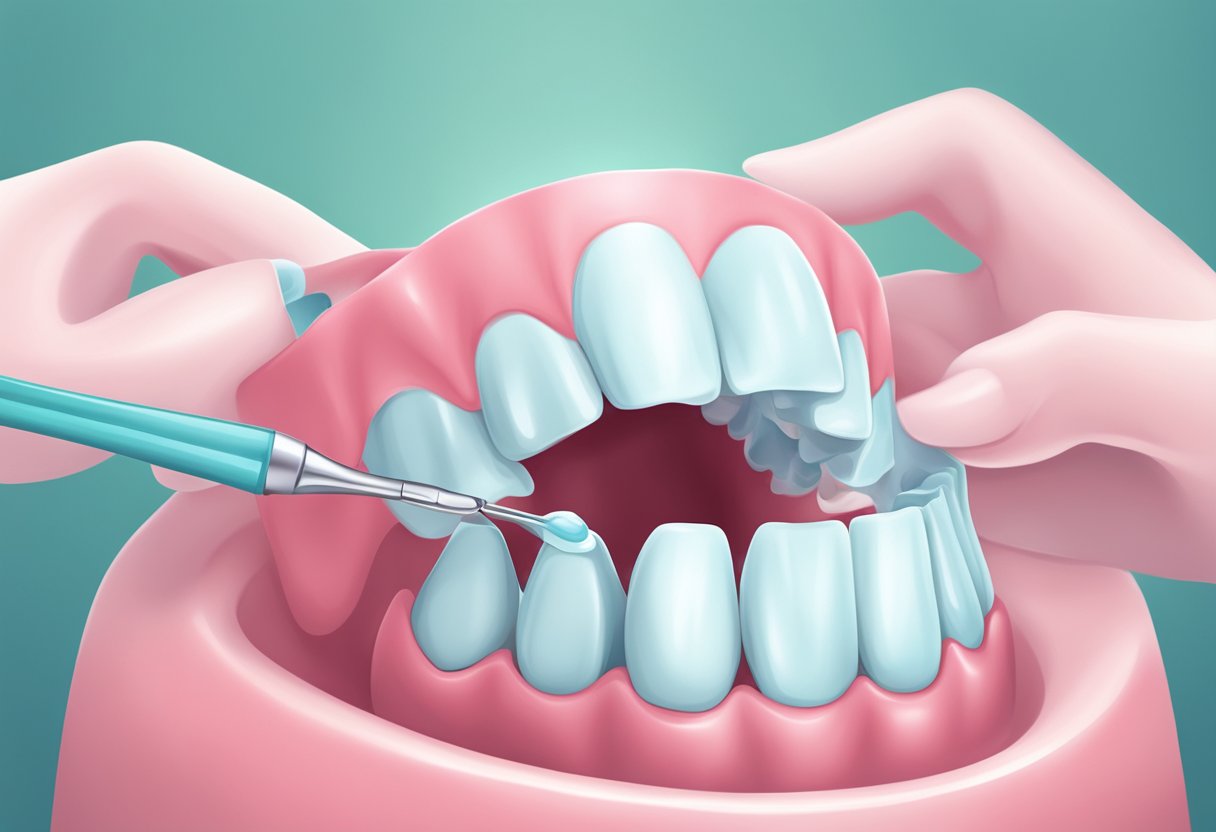
Dental Examination
During a dental examination, the dentist or periodontist visually inspects the patient’s mouth. This includes looking for signs of plaque and tartar buildup, inflammation, and gum recession. They use specialized instruments to probe the teeth and gums, checking for any abnormalities that indicate disease. Relevant medical history is also reviewed to identify any contributing factors to the patient’s symptoms, such as smoking or certain medications.
Gum Measurement
Measuring the deep pockets between the teeth and gums is a key part of the diagnosis. This is achieved using a periodontal probe, which helps the dentist gauge the depth of the spaces known as periodontal pockets. Healthy gums typically have pocket depths of 1 to 3 millimeters. Depths greater than 4 millimeters can be a sign of gum disease, with deeper pockets indicating more advanced disease states.
The results of the examination and measurements enable dental professionals to formulate an accurate diagnosis and develop an appropriate treatment plan.
Standard Treatments
The cornerstone of managing gum disease lies in thorough cleaning techniques and the appropriate use of medications. These treatments aim at reducing inflammation and infection to promote healing of the gums.
Scaling and Root Planing
Scaling and root planing are deep-cleaning procedures. Scaling involves removing plaque and tartar from the tooth surface and below the gumline. This can be performed using different tools such as a laser or an ultrasonic device. Root planing is a process where the roots of the teeth are smoothed out to help prevent tartar from reaccumulating and assist in the reattachment of the gums to the teeth.
Medication Use
Medications are often prescribed alongside mechanical cleaning procedures. Antibiotics such as doxycycline or minocycline might be used to help control bacterial infection. In some cases, a dentist may recommend an antibacterial mouthwash containing chlorhexidine to help reduce plaque and gingivitis. Triclosan, contained in some toothpastes, can also help reduce plaque and gingivitis.
Surgical Interventions
Surgical interventions for gum disease focus on access to deeper periodontal pockets and restoration of lost bone and tissue. These procedures are often necessary when a patient has advanced periodontitis where nonsurgical treatments like scaling and root planing are insufficient.
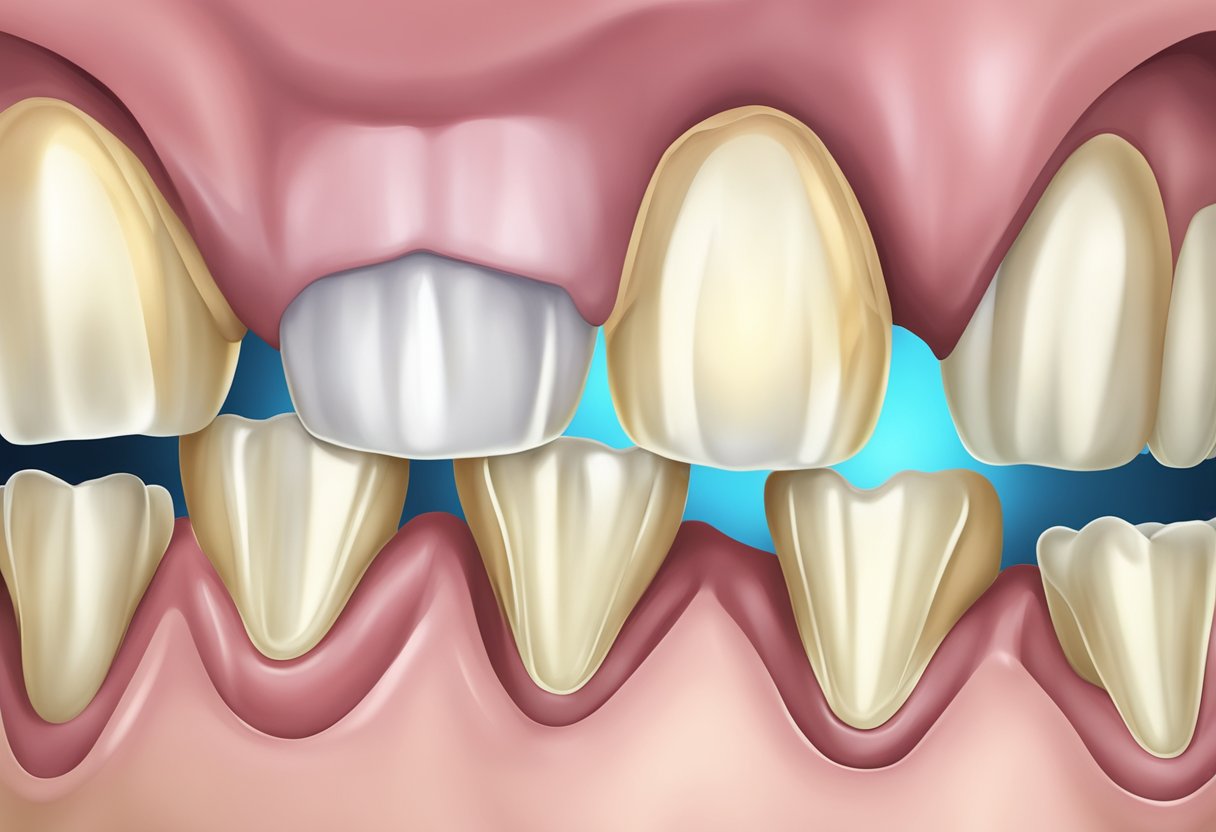
Flap Surgery
Flap surgery, or pocket reduction surgery, is a procedure where the gums are lifted back to remove tartar deposits in deep pockets. The gums are then sutured back in place to fit snugly around the tooth. This method aims to reduce the periodontal pocket and make it easier to keep the area clean.
Bone and Tissue Grafts
In cases of severe bone and tissue loss, bone grafting and soft tissue grafts may be recommended to regenerate lost tissue. Bone grafts involve placing natural or synthetic bone in the area of bone loss, which can be supplemented with guided tissue regeneration using a biocompatible membrane. Soft tissue grafts involve reinforcing thin gums or filling in places where gums have receded.
Daily Oral Hygiene Practices
Maintaining daily oral hygiene is essential for preventing gum disease. This includes specific practices such as thorough brushing, regular flossing, and the use of mouthwashes. Below, each foundational step is described to ensure that these practices are effective in sustaining oral health.
Toothbrushing Fundamentals
One should brush their teeth twice a day using fluoride toothpaste to remove dental plaque and prevent cavities. It is recommended to use a soft-bristled toothbrush and to brush for two minutes at a time, ensuring all tooth surfaces and the gum line are well-covered. Replace a toothbrush every three to four months or sooner if the bristles become frayed.
- Proper Technique:
- Angle the bristles at a 45-degree angle to the gums.
- Move the brush gently in short (tooth-wide) strokes.
- Brush outer, inner, and chewing surfaces of the teeth.
- Use vertical strokes for the inner surfaces of front teeth.
Flossing Routines
Daily flossing is crucial for removing plaque and food particles from between teeth where a toothbrush can’t reach. For best results, use an 18-inch strand of floss, winding most of it around one of the middle fingers and the rest around the opposite middle finger. Glide the floss between teeth with a gentle sawing motion.
- Effective Flossing Steps:
- Hold the floss tightly, allowing for controlled movements.
- Curve the floss around the base of each tooth, going beneath the gumline.
- Use clean sections of floss as you move from tooth to tooth.
Mouthwashes and Rinses
Using a mouthwash can be a helpful addition to manual brushing and flossing. Mouthwashes reduce oral bacteria and can contain fluoride to help prevent tooth decay. It’s important to use mouthwash as directed and not to substitute it for brushing and flossing. Swish the mouthwash in the mouth for 30 seconds to one minute, then spit it out.
- Choosing a Mouthwash:
- Look for an antiseptic mouthwash to reduce bacteria and plaque activity.
- Use fluoride mouthwashes to strengthen tooth enamel and protect against decay.
- Consider a mouthwash with specific ingredients if you have dry mouth or sensitive teeth.
Incorporating these key actions into one’s daily routine can significantly improve one’s oral hygiene and decrease the risk of gum disease. Techniques such as the proper use of an interdental brush can also complement these practices, especially for cleaning wider gaps. A diligent approach to oral care is the foundation of good oral health.
Lifestyle and Nutrition
Proper lifestyle choices and nutritional habits play a critical role in the healing and maintenance of gum health. Those suffering from gum disease may see significant improvements by adjusting their daily routines and diet.
Quitting Smoking and Tobacco
Smoking and tobacco use are among the most detrimental habits for oral health. They contribute to the onset and progression of gum disease by affecting blood flow to the gums and impairing the body’s immune response. Those who quit smoking can benefit from improved gum healing and a reduction in gum disease progression.
Dietary Choices and Supplements
A balanced diet rich in certain nutrients can support gum health. Foods high in Vitamin C, like citrus fruits and bell peppers, can strengthen the gums due to their collagen production-enhancing properties. Similarly, cranberry has been identified as beneficial due to its ability to prevent bacteria from sticking to the teeth and gums. In addition to a nutrient-dense diet, supplements containing calcium and Co-enzyme Q10 have been shown to support oral health. While not a dietary addition, the practice of oil pulling with substances like coconut oil might contribute to a reduction in bacteria and promote oral cleanliness. A consistent, nutrient-rich diet combined with a tobacco-free lifestyle is a comprehensive approach towards fighting gum disease.
Home Remedies and Natural Treatments
Home remedies and natural treatments can support oral care by addressing gum disease with ingredients such as tea tree oil and saltwater, which may offer antiseptic and healing properties. These remedies are to be used in conjunction with regular dental hygiene practices.
Tea Tree Oil
Tea Tree Oil is known for its natural anti-inflammatory and antimicrobial properties, which may make it beneficial in treating gum disease. A person can consider adding a drop of tea tree oil to their toothpaste before brushing, ensuring not to swallow the mixture, as tea tree oil is not for ingestion.
Saltwater Rinses
Saltwater rinses are a simple yet effective home remedy to reduce gum inflammation and cleanse the oral cavity. They advise dissolving one teaspoon of salt into a cup of warm water and swishing the solution in the mouth for 30 seconds. This saltwater rinse can be repeated several times a day to help promote healing and prevent bacterial growth.
Preventive Measures
Proper oral care and routine professional dental cleanings are foundational to preventing gum disease. These practices help mitigate the risk of developing periodontitis, ensuring that one’s oral health is maintained.
Regular Dental Visits
They are critical for maintaining oral health and preventing gum disease. Dental professionals recommend that individuals should undergo a dental examination and cleaning at least twice a year. During regular check-ups, dentists remove plaque and tartar buildup – a key step in preventing periodontitis.
- Professional Dental Cleanings: These are crucial as they can remove calcified deposits that regular brushing and flossing cannot.
- Personal Oral Care Routine: A dentist can also advise on proper brushing and flossing techniques to ensure effective at-home care.
Educational Awareness
Individuals should be informed about the importance of oral hygiene and its impact on overall health. Education on gum disease and its prevention can lead to better oral care practices.
- Knowledge of Gum Disease: Awareness about the causes and risks associated with periodontal disease can drive individuals to adopt a proactive approach to their oral health.
- Effective Oral Care Products: Dentists can provide recommendations on the most suitable products such as toothbrushes, toothpaste, and floss, tailored to each patient’s specific needs.
Complications of Gum Disease
Gum disease, if left unchecked, can lead to significant health issues beyond the mouth. These complications can range from tooth and bone damage to systemic health problems.
Impact on Overall Health
Research indicates that the inflammation associated with gum disease can be linked to a higher risk of heart disease. This oral condition might also increase the likelihood of stroke, diabetes, and respiratory diseases. There’s evidence suggesting associations between periodontitis and certain types of cancer, although more studies are necessary to understand these connections fully.
Tooth and Bone Damage
Periodontitis, an advanced form of gum disease, can lead to the destruction of the structures supporting teeth. This damage manifests not only as receding gums but also the loss of bone around the roots of teeth. As the condition worsens, tooth loss can occur. Additionally, the presence of persistent bad breath may serve as a warning for potential periodontal complications.
Advanced Care and Maintenance
When addressing gum disease, advanced care and maintenance are critical for healing and prevention of further complications. This approach typically requires professional intervention and a rigorous oral hygiene regimen.
Follow-up and Ongoing Treatment
After the initial treatment of gum disease, follow-up care with a periodontist is crucial to ensure the healing process is on track. They often recommend professional dental cleanings more frequently than the standard twice-yearly schedule. These cleanings help manage plaque and tartar that could otherwise exacerbate the condition. Patients may receive local anesthesia during these procedures to ensure comfort.
The periodontist may also evaluate the need for additional treatments like scaling and root planing or, in advanced cases, surgical interventions to reduce periodontal pockets. Ongoing treatment plans are tailored to the individual’s response to therapy and their specific requirements for gum disease management.
Long-Term Management
For long-term management of gum disease, maintenance revolves around steadfast oral hygiene practices. At home, patients are encouraged to adhere to a routine that includes:
- Twice-daily toothbrushing: Employing a soft-bristled toothbrush and fluoride toothpaste.
- Daily flossing: To clean the spaces between teeth where a toothbrush won’t reach.
- Antimicrobial mouthwash: As recommended by a dental professional to help reduce plaque.
Patients should also avoid lifestyle choices that negatively affect gum health, such as the use of tobacco products, which are known to impair healing. Regular check-ups with a periodontist are necessary to ensure that the gums remain healthy and to make any adjustments to the care plan as needed.
By combining professional care with diligent at-home maintenance, individuals can greatly enhance their chances of keeping their gums healthy and preventing the recurrence of gum disease.
Frequently Asked Questions
This section addresses common inquiries regarding gum disease, providing clear, evidence-based responses to assist individuals in recognizing symptoms, exploring treatment options, and understanding the disease’s progression.
What are the initial warning signs of gum disease?
The earliest signs of gum disease include bleeding gums, red or swollen gums, and persistent bad breath. These symptoms indicate the potential presence of gingivitis, the initial stage of gum disease.
How is gum disease effectively treated at home?
Effective home treatment for gum disease involves maintaining rigorous oral hygiene, such as regular brushing and flossing, to reduce plaque buildup. Using an antibacterial mouthwash can also help control the bacteria contributing to the disease.
Can surgical intervention improve severe cases of gum disease?
In severe cases, surgical intervention such as scaling and root planing can be performed to remove tartar and bacteria from beneath the gumline, and to help gums reattach to the teeth, improving the condition significantly.
What are the different stages of gum disease progression?
Gum disease progresses through multiple stages from gingivitis to advanced periodontitis. It starts with the inflammation of the gums and, if untreated, leads to gum recession, bone loss, and potentially tooth loss.
What underlying factors contribute to the development of gum disease?
Several factors can contribute to gum disease, including poor oral hygiene, smoking, diabetes, certain medications, and genetic susceptibility. These factors create conditions that allow plaque to build up and harden, leading to periodontal disease.
Is it possible to fully recover from gum disease and restore oral health?
It is possible to manage gum disease and restore oral health with prompt treatment, especially in the early stages. Consistent oral care routines and professional dental treatments are critical for recovery and preventing further damage.